
Public misconceptions about infectious diseases can be extremely dangerous. Many believe that when a person gets infected with a virus or bacteria, signs of infection are immediately felt or appear thereafter. This is particularly important in the current context of the pandemic.
Just like people who have COVID-19 and are asymptomatic, the reality is that many of us carry all types of bacteria without even knowing it—some are even born with them. In Quebec, 5-10% of healthy people are meningococcus carriers without even knowing it. ¹ If we’re lucky, we live out our lives as asymptomatic carriers and never experience meningitis or meningococcal blood infections caused by this bacterium. There are multiple types of meningococcus vaccines available, but not all are part of Quebec’s universal immunization program. ²
For the rest of Quebec’s population, catching meningococcus can cause serious health problems very quickly. Especially in those with pre-existing conditions, infants, or adolescents ³, having meningitis can require expensive long-term hospital stays and advanced treatments.
Rapid diagnostics increase accuracy and lower costs
When people enter a hospital and have meningitis without knowing it, rapid diagnostic solutions with a high accuracy rate (and those that test for other pathogens) are crucial for ensuring the best patient health outcomes and allowing staff to treat more patients daily. During the pandemic, it is more important than ever for hospitals to effectively manage the overflow of emergency rooms and free up beds.
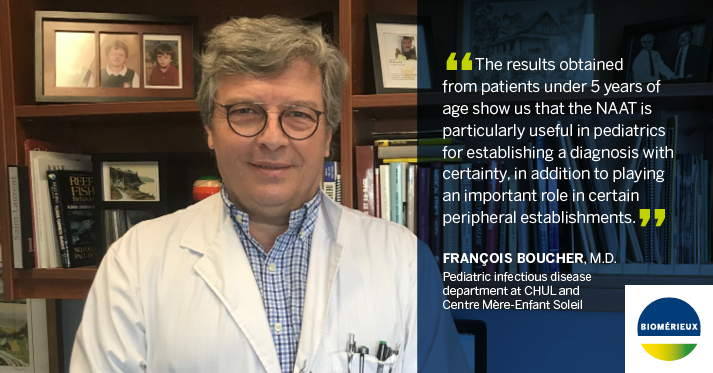
In a recent study, the pediatric team at CHU de Québec-Université Laval (CHUL) addressed how meningitis is diagnosed, citing that taking a bacterial culture of the cerebrospinal fluid (CSF) is not exactly accurate during preliminary stages of the disease, especially when the sample is taken after antibiotic therapy has begun. ³
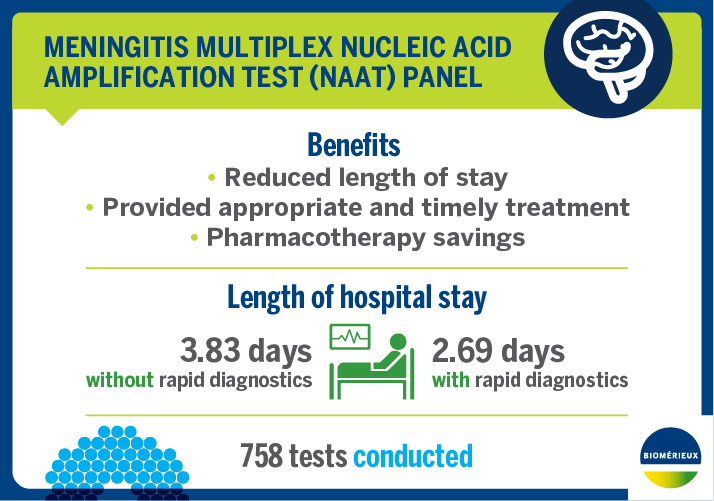
The CHUL pediatric team adopted a Meningitis multiplex nucleic acid amplification test (NAAT) panel and collected data findings over one year regarding its accuracy rate, ability to reduce hospital stay and cost of treatment.
Reducing hospital inpatient length of stay
A highlight of the study found that the multiplex NAAT panel reduced the length of hospital stay by one day in pediatrics, directly because of how quickly patients could be diagnosed. The presence of this rapid diagnostic solution enabled CHUL to free up hospital beds and discharge patients faster.
More patient-hospital benefits include pharmacotherapy savings in pediatrics, and better access to informed choice of treatment that provided a shorter response time with fast and highly effective patient care. Without early diagnosis and adequate treatment, 5-10% of patients die. ⁵ The lack of a universal immunization program makes it imperative to use the means necessary to administer the right treatment to each patient, especially in pediatrics, as quickly as possible.
You can download the PDF here.
REFERENCES
1) Government of Quebec, Meningococcal infections:
https://www.quebec.ca/en/health/health-issues/a-z/meningococcus/#:~:text=In%20Qu%C3%A9bec%2C%205%25%20to%2010,can%20cause%20meningitis%20or%20septicemia
2) Montreal Gazette, Here’s everything you need to know about meningitis (March 28, 2019): https://montrealgazette.com/news/local-news/heres-everything-you-need-to-know-about-meningitis
3) bioFire (website), The BioFire® FilmArray® Meningitis/Encephalitis (ME) Panel: https://www.biofiredx.com/products/the-filmarray-panels/filmarrayme/
4) Global News, Meningococcal B identified as strain that killed Montreal woman (March 26, 2019): https://globalnews.ca/news/5098675/meningococcal-b-strain-killed-montreal-woman/
5) World Health Organization Meningococcal meningitis (February 2018): https://www.who.int/fr/news-room/fact-sheets/detail/meningococcal-meningitis
Leave a Reply